Few biological systems remain as enigmatic—and as critical to human survival—as the placenta. This temporary organ is the lifeline between mother and child, orchestrating the exchange of nutrients, oxygen, and hormones during pregnancy. When it works well, life thrives. When it malfunctions, the results can be devastating, leading to hundreds of thousands of maternal deaths and millions of infant deaths worldwide each year.
For decades, scientists have struggled to study the placenta during its earliest, most formative stages. By the time a pregnancy reaches full term, the placenta has already transformed so dramatically that it no longer reflects its early biology. Obtaining first-trimester tissue is nearly impossible without endangering the pregnancy. Animal models, meanwhile, fail to capture the uniquely human complexity of this organ.
But now, researchers at the University of Technology Sydney (UTS) have turned to an unexpected tool—3D bioprinting—to create miniature, lab-grown placentas that mimic the earliest stages of human development. Their work, published in Nature Communications, could open an entirely new chapter in maternal-fetal medicine.
Printing the Unprintable
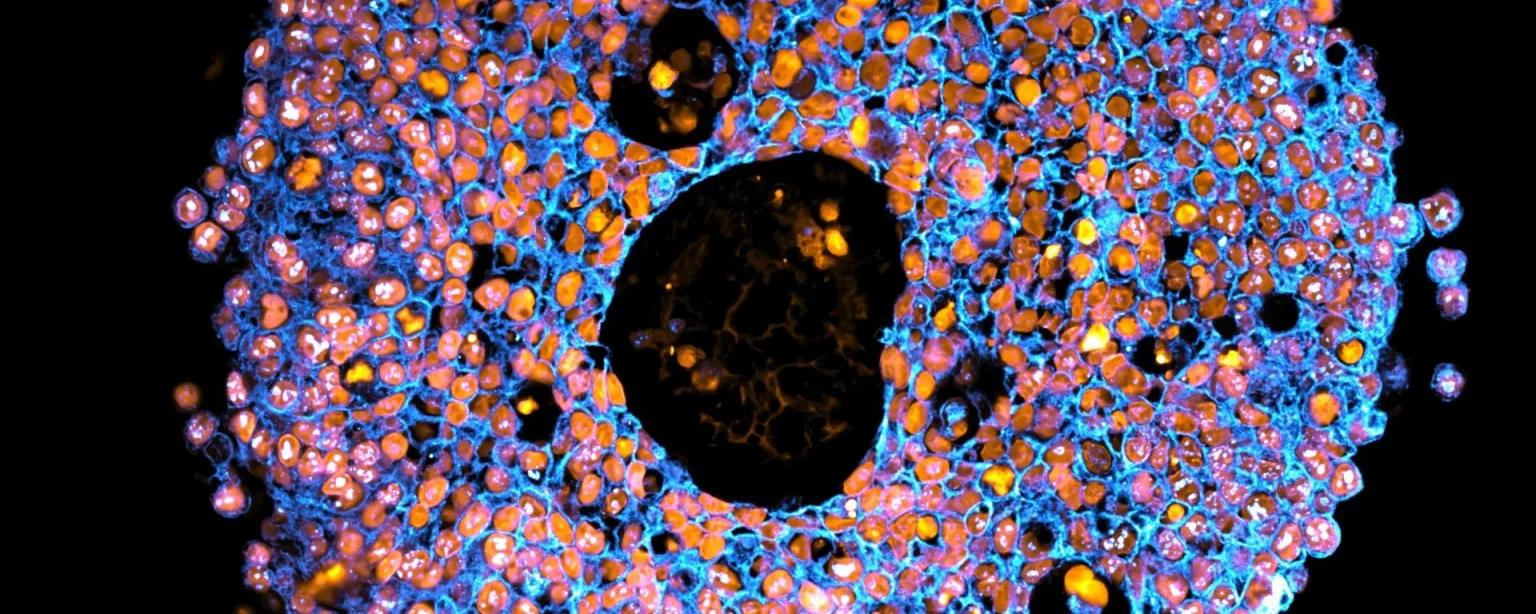
The UTS team began with trophoblasts, the specialized cells that form the outer layer of the placenta. Using a synthetic, tunable gel and precise bioprinting techniques similar to inkjet printing, they deposited droplets of these cells into culture plates. Over time, the cells organized themselves into placental organoids—tiny, functional replicas of the organ’s structure.
When compared with organoids created through traditional manual methods, the bioprinted versions proved more accurate in their representation of early placental tissue. They showed distinct differences in how subtypes of trophoblasts developed and how closely they matched actual human tissue samples.
This difference matters. By controlling the microenvironment with precision, scientists can replicate the subtle cues that shape how cells mature and function. What emerges is a laboratory model of pregnancy’s earliest mysteries—one that is safer, more scalable, and more faithful to human biology than anything we’ve had before.
Cracking the Code of Preeclampsia
One of the most promising aspects of this research is its potential to illuminate preeclampsia, a pregnancy complication that has baffled medicine for centuries. Characterized by high blood pressure, organ dysfunction, and severe risks to both mother and baby, preeclampsia remains unpredictable and poorly understood.
The UTS team exposed their printed placental organoids to inflammatory molecules that are elevated in women with preeclampsia. The organoids reacted in ways that mirrored the disease, creating a testbed for new therapies. Researchers were able to observe how potential drugs influenced placental development in real time—something previously impossible without endangering patients.
This is more than an academic exercise. It’s the foundation for a future in which pregnancy complications could be predicted, prevented, and treated long before they spiral into crisis.
The Bigger Picture: A New Era of Bioprinting
While this research focuses on pregnancy, its implications stretch much further. 3D bioprinting is rapidly emerging as one of the most transformative tools in medicine. Scientists are already experimenting with printing liver tissue for drug testing, skin grafts for burn victims, and even early prototypes of vascularized organs. The placenta may be one of the most difficult biological puzzles we’ve faced, but solving it demonstrates the sheer versatility of this technology.
Imagine a world where bioprinted models replace animal testing entirely. Where complex human diseases can be studied in organoids that faithfully mimic their tissue of origin. Where treatments are tested on printed models of a patient’s own biology before being delivered. This is not just the future of pregnancy research—it’s the future of personalized medicine.
Ethical and Social Implications
The ability to bioprint the placenta raises profound questions. Could we one day grow a full placenta outside the body to support high-risk pregnancies? Could organoid-based testing become a standard prenatal screening tool, predicting risks before they manifest? What happens when the boundaries between natural gestation and engineered support begin to blur?
These questions will challenge our definitions of motherhood, family, and medical intervention. As with all radical technologies, society will need to grapple not just with what we can do, but with what we should do.
Final Thoughts
The placenta is often overlooked, discarded after birth as though its purpose is complete. Yet it is one of the most intricate and essential organs humanity has ever known. By recreating it in the lab with 3D bioprinting, scientists are not just solving a medical puzzle—they are rewriting our understanding of life itself.
This breakthrough hints at a future where no pregnancy complication is a mystery, where maternal deaths plummet, and where medicine can intervene with precision long before crises arise. The ability to bioprint life’s earliest connections is not just science—it is a glimpse into a future where humanity takes an unprecedented role in shaping its own survival.
Read more on related topics:
- How 3D Bioprinting Is Redefining the Future of Medicine
- The Next Frontier of Organ Printing and Regenerative Healthcare