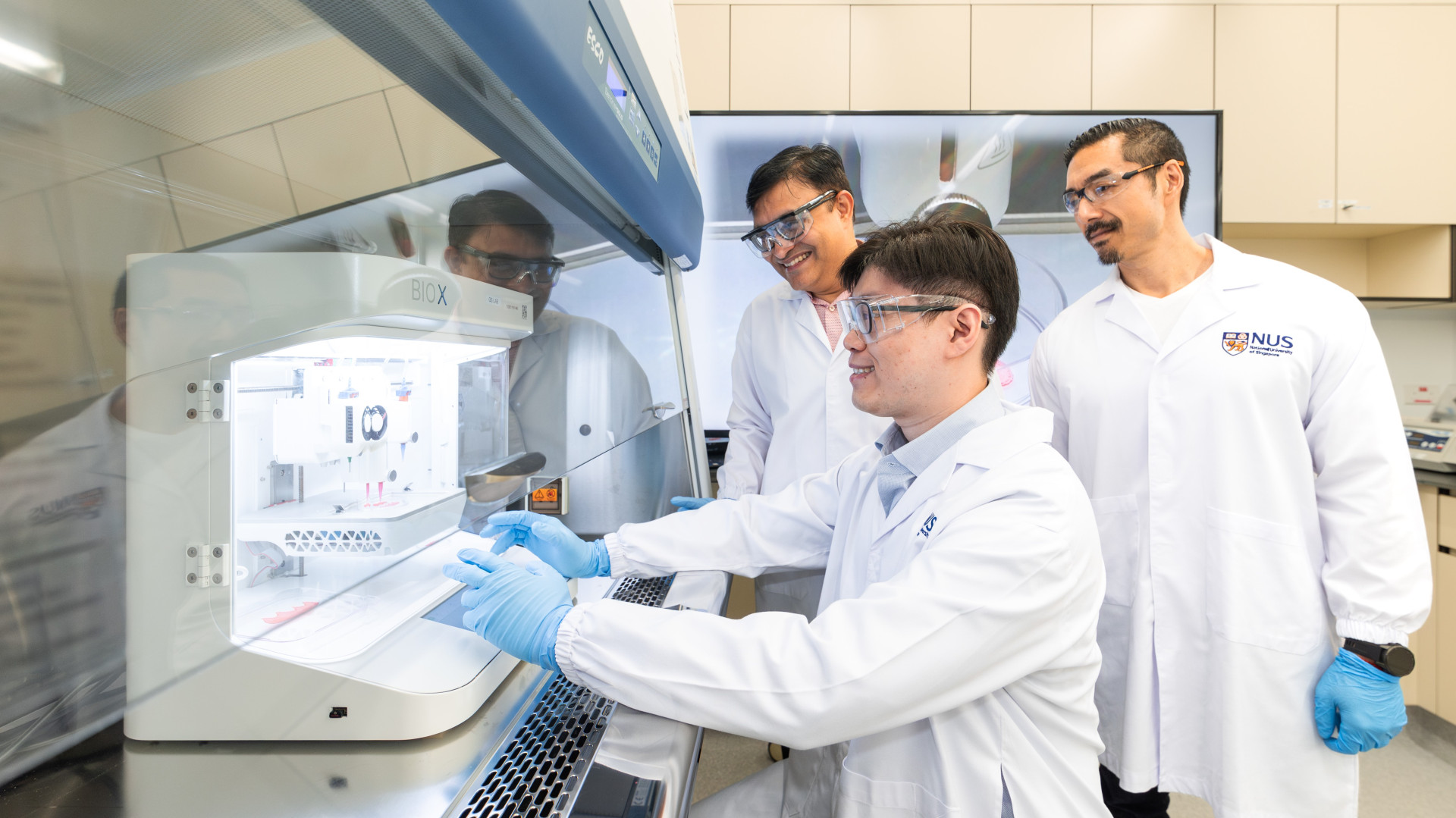
A team of researchers from the National University of Singapore (NUS) has developed a groundbreaking technique that combines 3D bioprinting with artificial intelligence (AI) to produce personalized gum grafts, offering a less invasive alternative to traditional dental surgery. Led by Assistant Professor Gopu Sriram from the NUS Faculty of Dentistry, this innovation aims to reduce patient discomfort by eliminating the need to harvest tissue from the patient’s own mouth—a common and often painful step in current grafting procedures.
Designed for use in treating gum defects caused by periodontal disease or complications from dental implants, the team’s approach relies on a specially formulated bio-ink that supports cell growth while maintaining the mechanical strength necessary during the 3D printing process. Their research, published in Advanced Healthcare Materials on December 17, 2024, was funded by the National Additive Manufacturing Innovation Cluster and the National University Health System.
One of the standout features of this work is the integration of AI into the bioprinting workflow. “To speed up the 3D bioprinting process, we integrated AI into our workflow to address this critical bottleneck,” said Professor Dean Ho, Head of the Department of Biomedical Engineering at NUS and co-corresponding author. By using machine learning algorithms, the team drastically reduced the number of experiments needed to fine-tune bioprinting parameters—from potentially thousands to just 25. This dramatically increased efficiency while maintaining accuracy and quality.
Assistant Professor Sriram emphasized the complexity of this achievement: “Our study is among the first to specifically integrate 3D bioprinting and AI technologies for the biofabrication of customized oral soft tissue constructs. Bioprinting is far more challenging than conventional 3D printing because it involves living cells, which adds multiple layers of complexity to the process.”
The results have been impressive. The bioprinted grafts showed over 90% cell viability immediately after printing and maintained that high rate throughout an 18-day culture period. Importantly, the technology enables the fabrication of grafts tailored precisely to a patient’s wound dimensions. “This precision reduces or even eliminates the need for tissue harvesting, lowering surgery time, discomfort, and the risk of complications,” added Dr. Jacob Chew, a periodontist and co-investigator of the study. “It also helps minimize graft distortion and tension during wound closure, improving clinical outcomes.”
Looking ahead, the research team plans to conduct in vivo studies to evaluate how well the grafts integrate and remain stable in the oral environment. They are also exploring multi-material bioprinting to integrate blood vessels into future constructs, which would support even more complex tissue engineering applications.
This innovative approach could transform regenerative dentistry and pave the way for broader applications in tissue engineering and personalized medicine—bringing us closer to a future where dental grafts are custom-printed, cell-friendly, and surgery-free.
By Impact Lab