Researchers at the University of California, San Diego (UCSD) have unveiled a groundbreaking wearable ultrasound patch designed for continuous, noninvasive blood pressure monitoring. This innovative device is the first of its kind to undergo extensive clinical validation on over 100 patients, offering a new and potentially transformative method for tracking cardiovascular health both in clinical settings and at home. The results of the study were recently published in Nature Biomedical Engineering.
Traditional blood pressure measurements, such as those taken with a cuff, typically provide only one-time readings, which can miss important trends and fluctuations. In contrast, the UCSD-developed wearable patch continuously monitors blood pressure and provides real-time waveform data, offering detailed insights into changes and trends over time. According to Sai Zhou, co-first author of the study and recent Ph.D. graduate from the UCSD Jacobs School of Engineering, this continuous data stream allows for better monitoring of cardiovascular health.
“This wearable patch offers a continuous stream of blood pressure waveform data, allowing it to reveal detailed trends in blood pressure fluctuations that are often missed by traditional, one-time cuff measurements,” Zhou explained.
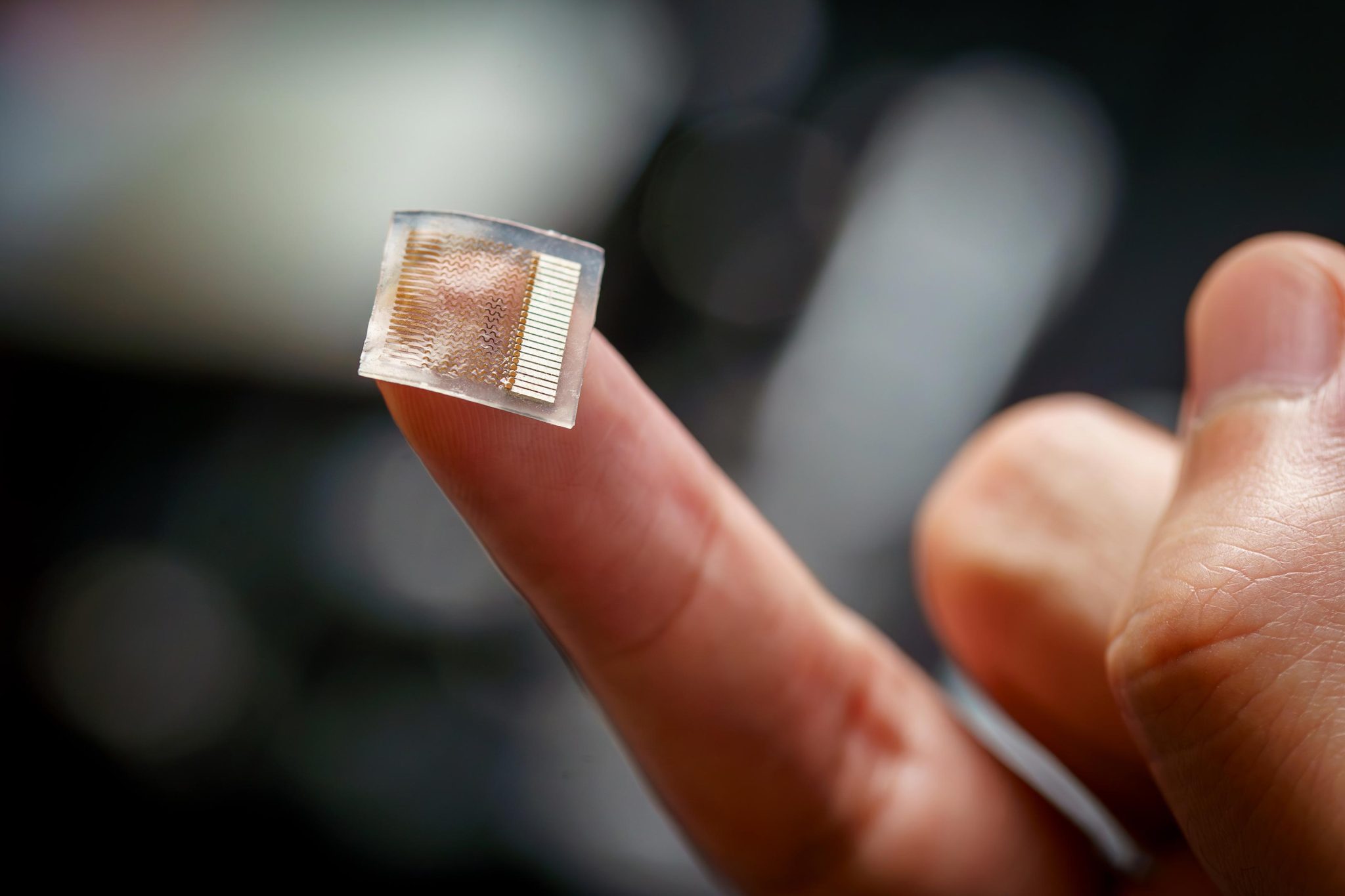
The patch is a soft, stretchy device about the size of a postage stamp that adheres to the skin, typically worn on the forearm. Made of a flexible silicone elastomer, the patch contains an array of small piezoelectric transducers sandwiched between stretchable copper electrodes. These transducers emit and receive ultrasound waves that track changes in the diameter of blood vessels, which are then converted into accurate blood pressure readings.
The wearable ultrasound patch builds on an earlier prototype developed by Sheng Xu, a professor in UCSD’s Aiiso Yufeng Li Family Department of Chemical and Nano Engineering. The team made two key improvements to enhance the device’s functionality for continuous blood pressure monitoring:
- Improved Transducer Design: The piezoelectric transducers were packed closer together, expanding their coverage to target smaller arteries, such as the brachial and radial arteries, which are crucial for accurate blood pressure monitoring.
- Enhanced Signal Clarity: A backing layer was added to dampen redundant vibrations from the transducers, improving the clarity of the signal and the accuracy of tracking the arterial walls.
The patch has undergone rigorous testing, with results that closely align with traditional blood pressure cuffs and other invasive devices, such as the arterial line—a sensor placed directly in an artery for continuous blood pressure measurement. While the arterial line is the gold standard in intensive care units (ICUs) and operating rooms, it is invasive, uncomfortable, and limits patient mobility. In contrast, the ultrasound patch provides a noninvasive, comfortable, and reliable alternative.
The patch was tested on a total of 117 subjects across various settings. In one set of tests, seven participants wore the patch during daily activities, including cycling, eating, mental arithmetic, and consuming energy drinks. In a larger cohort of 85 subjects, the patch was tested during posture changes, such as transitioning from sitting to standing. In all tests, the patch’s readings closely matched those of traditional blood pressure cuffs.
The patch was also evaluated in clinical settings. In a cardiac catheterization laboratory, 21 patients wore the patch while undergoing procedures, and four ICU patients wore it after surgery. The results from the wearable ultrasound patch were in close agreement with the measurements taken from the arterial line, underscoring its potential as a noninvasive alternative for continuous blood pressure monitoring.
One of the major advances of this technology is the thorough clinical validation it underwent, which was critical for ensuring its accuracy across a variety of real-world settings. As Xu noted, factors like “white coat syndrome,” masked hypertension, daily activities, and medications can cause blood pressure to fluctuate, making it challenging to get an accurate diagnosis and effectively manage treatment. By testing the device in a wide variety of real-world and clinical scenarios, the research team ensured the device’s reliability under various conditions, which is often skipped in other wearable device studies.
“We made sure to test this device thoroughly in real-world and clinical settings. Many studies on wearable devices don’t go to this length, but we wanted to ensure the patch could work reliably for all patients,” Xu said.
The team at UCSD is already preparing for large-scale clinical trials and aims to integrate machine learning to further enhance the patch’s capabilities. There are also ongoing efforts to develop a wireless, battery-powered version of the device for long-term use, as well as seamless integration with hospital systems. The technology has the potential to revolutionize how blood pressure is monitored, offering a noninvasive, continuous, and more accurate alternative to traditional methods, making it easier for both patients and healthcare providers to track cardiovascular health.
This wearable ultrasound patch not only offers a promising tool for better blood pressure monitoring but also paves the way for future innovations in wearable health technology, providing new insights into patient care, diagnostics, and treatment management.
By Impact Lab