Australia has made a groundbreaking leap in medical technology with the successful implantation of the nation’s first durable artificial heart. This revolutionary device, the BiVACOR Total Artificial Heart, was implanted in a patient in Sydney last November, making him the world’s first person to be discharged from a hospital with the high-tech device still in place.
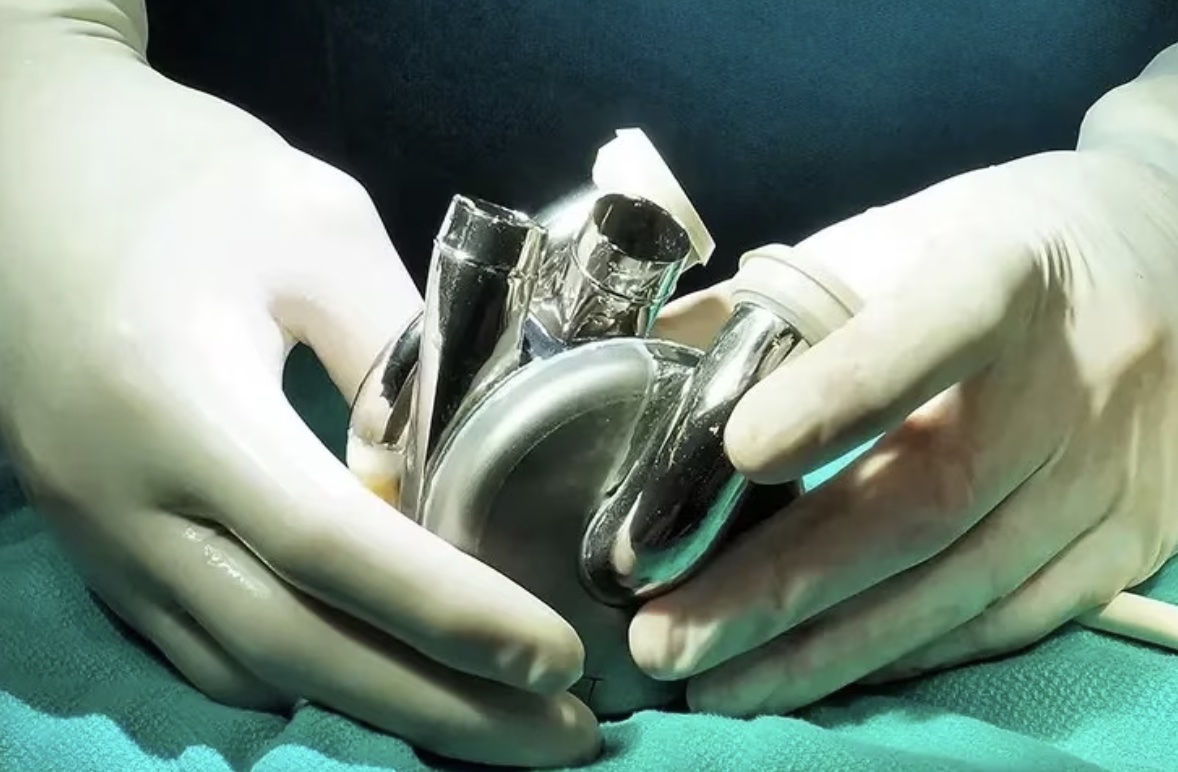
During a six-hour procedure at St Vincent’s Hospital, surgeons implanted the BiVACOR, a titanium-based mechanical blood pump, into a man suffering from severe heart failure. Initially, the implant was intended as a temporary solution until a donor heart became available. However, the long-term vision for BiVACOR is to offer a permanent alternative to heart transplantation, potentially eliminating the need for heart donors altogether.
The operation, led by renowned cardiothoracic and transplant surgeon Dr. Paul Jansz, was described as an emotional milestone. Dr. Jansz confessed to feeling “goosebumps” when inventor Daniel Timms switched on the artificial heart for the first time. Timms, the Queensland-born innovator behind the device, has dedicated years to perfecting the BiVACOR, which is designed to avoid mechanical failure or rejection by the body.
The BiVACOR uses a motor to pump blood throughout the body, but unlike traditional mechanical pumps, it uses magnets to suspend the rotor, preventing wear and tear from friction. This design makes the device far more durable than its predecessors, offering a promising solution for those in need of heart transplants.
Daniel Timms’ passion for creating the artificial heart started in his childhood, when he would spend hours tinkering with water pumps alongside his plumber father. This interest would eventually grow into a lifelong commitment to solving the problem of heart failure. Timms’ father passed away from heart failure, which only fueled his determination to finish what he had started.
“Growing up, we had a goal – could we get the biggest receipt at Bunnings?” Timms recalled. “We’d buy everything we could to make progress on the project.” His efforts have now culminated in the BiVACOR, a device that Timms hopes will benefit Australians long before it reaches international markets.
The patient who received the implant, a man in his 40s from New South Wales, had been critically ill prior to the surgery. His condition was so severe that he could barely walk to the bathroom, and his chances of surviving long enough to receive a donor heart were slim. After being implanted with the BiVACOR, he lived with the artificial heart for over 100 days until a matching donor heart was found.
Timms expects that within the next two to three years, the BiVACOR will no longer be a novelty but a common option for heart failure patients. “We just need to ramp up production,” he said. “We’re making more devices now, so they’ll be ready and waiting.”
In 2024, the BiVACOR was first implanted in a patient at the Texas Heart Institute, though that patient did not survive long enough to be discharged. Since then, four additional patients in the U.S. have received the implant, but none were discharged with the device in place. The BiVACOR’s battery lasts four hours before requiring a change, and there are hopes that future iterations will eliminate the need for patients to carry a battery pack, possibly using wireless charging technology instead.
The success of this historic surgery was particularly poignant as it took place at St Vincent’s Hospital, the same location where Australia’s first-ever heart transplant was performed in 1968. Notably, Australia’s first successful heart transplant took place there in 1984, performed by the legendary Victor Chang.
Looking ahead, doctors at Melbourne’s Alfred Hospital are currently undergoing training to implant BiVACOR devices, with the first procedure expected around mid-2025.
Heart failure claims the lives of approximately 5,000 Australians each year. While it can develop gradually, it often leads to a reduced ability of the heart to pump blood, causing debilitating effects. The BiVACOR device offers hope for patients who cannot wait for a donor heart or for those in areas where organ donations are scarce.
Australia is facing a critical shortage of organ donors, with a 5% drop in the number of transplant recipients last year, and heart transplants alone down by 19%. Cardiologist Dr. Chris Hayward of St Vincent’s Hospital emphasized that the BiVACOR artificial heart could become an essential solution for patients unable to wait for a donor heart.
This innovative device represents a giant leap forward in heart failure treatment, and with increased manufacturing and further testing, it could one day save the lives of countless patients in need.
By Impact Lab